Substance Use Disorders, Addiction, and Dependence
| 1. Addictive Qualities of Popular Drugs
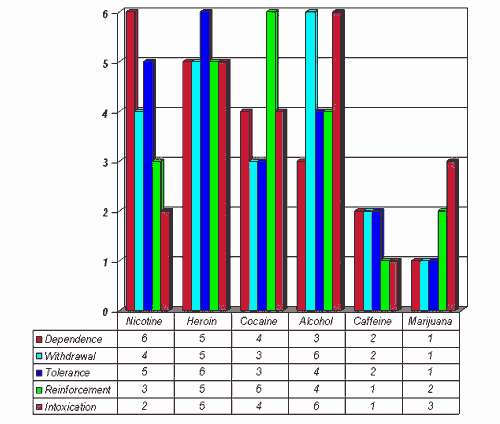
In 1994, for an article in the New York Times, Dr. Jack E. Henningfield of the National Institute on Drug Abuse and Dr. Neal L. Benowitz of the University of California at San Francisco ranked six substances based on five problem areas. Withdrawal: Presence and severity of characteristic withdrawal symptoms. Reinforcement: A measure of the substance's ability, in human and animal tests, to get users to take it again and again, and in preference to other substances. Tolerance: How much of the substance is needed to satisfy increasing cravings for it, and the level of stable need that is eventually reached. Dependence: How difficult it is for the user to quit, the relapse rate, the percentage of people who eventually become dependent, the rating users give their own need for the substance and the degree to which the substance will be used in the face of evidence that it causes harm. Intoxication: Though not usually counted as a measure of addiction in itself, the level of intoxication is associated with addiction and increases the personal and social damage a substance may do. "Is Nicotine Addictive? It Depends on Whose Criteria You Use." New York Times, Aug. 2, 1994. |
| 2. General Criteria for Drug Dependence, Including Nicotine Dependence "The 1988 Surgeon General’s report lists the following general 'criteria for drug dependence,' including nicotine dependence (USDHHS 1988, p. 7): "Primary Criteria "Additional Criteria "These criteria are consistent with those for a diagnosis of dependence provided in the Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV) (American Psychiatric Association [APA] 2000) and the International Classification of Diseases, Tenth Revision (ICD-10) (Table 4.1) (World Health Organization [WHO] 1992). The diagnosis of dependence using these diagnostic systems depends on the person experiencing a specific number of these symptoms. The relevance of some of these symptoms to nicotine addiction may be questionable because the DSM criteria are used across different drugs of abuse. For example, one symptom of addiction is that a great deal of time is spent in activities necessary to obtain the substance or recover from its effect. This criterion may not be as relevant to the diagnosis of nicotine addiction compared with other abused substances." US Department of Health and Human Services. "How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General." Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2010, pp. 105-106. |
| 3. Estimated Number Of People In The US Who May Have A Substance Use Disorder "In 2023, 48.5 million people aged 12 or older (or 17.1 percent of the population) had an SUD [Substance Use Disorder] in the past year, including 28.9 million people who had an alcohol use disorder and 27.2 million people who had a drug use disorder (Figures 28, 29, and 30 and Tables A.15B and A.16AB). People who had an SUD in the past year tended to have an alcohol use disorder only or a drug use disorder only. About 1 in 6 people with a past year SUD (15.6 percent or 7.5 million people) had both an alcohol use disorder and a drug use disorder in the past year. "The percentage of people aged 12 or older in 2023 with a past year SUD differed by age group. The percentage was highest among young adults aged 18 to 25 (27.1 percent or 9.2 million people), followed by adults aged 26 or older (16.6 percent or 37.0 million people), then by adolescents aged 12 to 17 (8.5 percent or 2.2 million people) (Figure 30 and Table A.15B). "By Race/Ethnicity "The percentage of people aged 12 or older in 2023 with a past year SUD was higher among American Indian or Alaska Native (25.3 percent), Multiracial (24.3 percent), or White people (17.8 percent) compared with Hispanic (15.7 percent) or Asian people (9.2 percent) (Figure 31 and Table B.13B). Multiracial people were also more likely than White or Black people (17.6 percent) to have had a past year SUD. Asian people were less likely to have had a past year SUD than people in other racial or ethnic groups. The percentage of people aged 12 or older in 2023 with a past year SUD could not be calculated with sufficient precision for Native Hawaiian or Other Pacific Islander people.15 Substance Abuse and Mental Health Services Administration. (2024). Key substance use and mental health indicators in the United States: Results from the 2023 National Survey on Drug Use and Health (HHS Publication No. PEP24-07-021, NSDUH Series H-59). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. |
| 4. Brain Disease Model of Addiction "In 1997, Alan Leshner, the Director of the US National Institute on Drug Abuse (NIDA), proclaimed that addiction was a chronic, relapsing, brain disease (Leshner, 1997). According to Leshner, drug use begins as a voluntary act but when drug use becomes regular and heavy, a neurochemical switch in the brain makes it very difficult to for the person to stop using drugs, despite their best efforts to do so. This has been called the brain disease model of addiction (BDMA). "Leshner and others argued that broad societal acceptance of the BDMA would deliver more effective addiction treatments that health insurers would fund and make more accessible to persons with addictions (Volkow and Li, 2004, Dackis and O’Brien, 2005, Leshner, 1997). They also predicted that the BDMA would reduce stigma because the public would accept that persons with an addiction had a brain disease that was in need of treatment rather than punishment (Volkow, 2015)." Hall W, Gartner C, Morphett K. How has the brain disease model of addiction contributed to tobacco control?. Drug Alcohol Depend. 2023;253:111033. doi:10.1016/j.drugalcdep.2023.111033 |
| 5. How SAMHSA Comes Up With Its Estimate Of The Prevalence Of "Illicit Drug Use Disorders" For The NSDUH "Illicit drug use disorder is defined as meeting DSM-IV criteria for either dependence or abuse for one or more of the following illicit drugs: marijuana, cocaine, heroin, hallucinogens, inhalants, methamphetamine, or prescription psychotherapeutic drugs that were misused (i.e., pain relievers, tranquilizers, stimulants, and sedatives). There are seven possible dependence criteria for specific illicit drugs: "1. spent a lot of time engaging in activities related to use of the drug, "For most illicit drugs, dependence is defined as meeting three or more of these seven criteria. However, experiencing withdrawal symptoms is not included as a criterion for some illicit drugs based on DSM-IV criteria. For these substances, dependence is defined as meeting three or more of the first six criteria. "Respondents who used (or misused) a specific illicit drug in the past 12 months and did not meet the dependence criteria for that drug were defined as having abuse were defined as meeting the abuse criteria for that drug if they reported one or more of the following: "1. problems at work, home, and school because of use of the drug; "Application of these criteria is discussed briefly in the respective SUD sections for specific illicit drugs. Detailed definitions for SUDs for specific illicit drugs also can be found in a glossary of key definitions for the 2016 NSDUH.9" Substance Abuse and Mental Health Services Administration. (2017). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. |
| 6. Proportion of Clients in Treatment in the US for Alcohol Alone, Other Substances Alone, or In Combination "The proportion of clients in treatment for the three broad categories of substance abuse problems—both alcohol and drug abuse, drug abuse alone, and alcohol abuse alone—demonstrated some changes between 2011 and 2020. "● The percentage of clients in treatment for both drug and alcohol abuse decreased from 44 percent in 2011 to 31 percent in 2020. (The number of clients in treatment for both drug and alcohol abuse decreased from 535,258 in 2011 to 333,526 in 2020 [Table 3.3].) "● The percentage of clients in treatment for drug abuse alone increased from 38 percent in 2011 to 52 percent in 2020. (The number of clients in treatment for drug abuse alone increased from 464,406 in 2011 to 743,828 in 2019 and then decreased to 569,522 in 2020 [Table 3.3].) "● The percentage of all clients in treatment for alcohol abuse alone decreased from 18 percent in 2009 to 13 percent in 2020. (The number of clients in treatment for alcohol abuse alone decreased from 221,632 in 2011 to 146,710 in 2020 [Table 3.3].) "● The percentage of clients in treatment for diagnosed co-occurring mental and substance use disorders increased from 41 percent in 2011 to 49 percent in 2020. (The number of clients in treatment for diagnosed co-occurring mental and substance use disorders increased from 506,162 in 2011 to 702,914 in 2019, before falling to 531,105 in 2020 [Table 3.3].)" Substance Abuse and Mental Health Services Administration, National Survey of Substance Abuse Treatment Services (N-SSATS): 2020. Data on Substance Abuse Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2021. |
| 7. Addictive Potential Of Various Drugs Including Marijuana, Heroin, Amphetamines, LSD "Of the people who sample a particular substance, what portion will become physiologically or psychologically dependent on the drug for some period of time? Heroin and methamphetamine are the most addictive by this measure. Cocaine, pentobarbital (a fast-acting sedative), nicotine and alcohol are next, followed by marijuana and possibly caffeine. Some hallucinogens—notably LSD, mescaline and psilocybin—have little or no potential for creating dependence." Gable, Robert S., "The Toxicity of Recreational Drugs," American Scientist (Research Triangle Park, NC: Sigma Xi, The Scientific Research Society, May-June 2006) Vol. 94, No. 3, p. 208. |
| 8. Development of Substance Use Disorders By Adolescents Estimated Using NSDUH Data "The prevalence of lifetime substance use among adolescents in 2018 was 26.3% (95% CI, 25.4-27.2) for alcohol, 15.4% (95% CI, 14.7-16.1) for cannabis, and 13.4% (95% CI, 12.7-14.1) for tobacco; among young adults in 2018, prevalence of lifetime substance use was 79.7% (95% CI, 78.9- 80.5) for alcohol, 51.5% (95% CI, 50.4-52.6) for cannabis, and 5.0% (95% CI, 53.9-56.1) for tobacco. Prevalence of SUDs differed by substance, age group, and time since initiation. Adjusted prevalence of cannabis use disorder was higher among adolescents than among young adults within 12 months of initiation (10.7%; 95% CI, 9.3-12.3 vs. 6.4%; 95% CI, 5.2-7.9) and at more than 36 months (20.1% [95% CI, 18.0-22.3] vs. 10.9% [95% CI, 10.3-11.4]) (Table). Prevalence of alcohol use disorder and nicotine dependence did not differ between the 2 groups within 12 months of initiation but was higher for young adults in subsequent periods. "Among young adults, prevalence of lifetime cocaine, methamphetamine, and heroin use in 2018 was 11.4% (95% CI, 10.7-12.1), 2.5% (95% CI, 2.2-2.8), and 1.3% (95% CI, 1.1-1.5), respectively. Within 12 months of initiation, adjusted prevalence was higher for methamphetamine use disorder (24.8% [95% CI, 16.8-34.9]) and heroin use disorder (30.9% [95% CI, 20.6-43.4]) than for cocaine use disorder (5.6% [95% CI, 4.2-7.4]). Estimates for adolescents were not reported owing to limited samples. "Prevalence of lifetime misuse of prescription drugs in 2014 was 9.2% (95% CI, 8.7-9.7) among adolescents and 26.3% (95% CI, 25.4-27.2) among young adults. Among the population with lifetime misuse, adjusted prevalence of prescription opioid use disorder, prescription stimulant use disorder, and prescription tranquilizer use disorder were consistently higher for adolescents than for young adults (Figure). Prevalence since time of initiation for adolescents was stable for prescription opioid use disorder and decreased for prescription stimulant use disorder and prescription tranquilizer use disorder, whereas for young adults, prevalence increased for prescription opioid use disorder and was stable for prescription stimulant use disorder and prescription tranquilizer use disorder." Volkow ND, Han B, Einstein EB, Compton WM. Prevalence of Substance Use Disorders by Time Since First Substance Use Among Young People in the US. JAMA Pediatr. Published online March 29, 2021. doi:10.1001/jamapediatrics.2020.6981 |
| 9. Low Prevalence of Alcohol Dependence Among US Adult Drinkers "This study found that about 9 of 10 adult excessive drinkers did not meet the diagnostic criteria for alcohol dependence. About 90% of the adults who drank excessively reported binge drinking, and the prevalence of alcohol dependence was similar among excessive drinkers and binge drinkers across most sociodemographic groups. The prevalence of alcohol dependence also increased with the frequency of binge drinking. However, even among those who reported binge drinking 10 or more times in the past month, more than two-thirds did not meet diagnostic criteria for alcohol dependence according to their responses to the survey. "The prevalence of alcohol dependence among adult excessive drinkers and binge drinkers in this study was slightly higher than the prevalence reported in other studies using the same diagnostic criteria for the classification of alcohol dependence. A 2001 study of alcohol abuse and dependence among US adults using the National Household Survey on Drug Abuse (NHSDA) — the precursor to the NSDUH — found that the prevalence of alcohol dependence was 7.4% among men and 7.3% among women who reported binge drinking (13). The higher prevalence of alcohol dependence among binge drinkers in this study may be due to the different time period as well as differences in the survey methods, which make these estimates not directly comparable (14). The former NHSDA was redesigned in 1999, and other changes were made to the survey in 2002, which may have increased the sensitivity of the NSDUH for identifying people who are binge drinking and alcohol dependent. "Differences in the prevalence of alcohol dependence between the current study and the 2002 study in New Mexico (10.7% among excessive drinkers and 8.1% among binge drinkers) (8) are probably due to differences in the survey methods used by the NSDUH and the BRFSS as well as differences in the populations studied (15). "Consistent with previous studies, binge drinking was most common among men, those aged 18 to 24, non-Hispanics whites, those with some college education, and those with an annual family income $75,000 or more (16). In contrast, alcohol dependence was most common among American Indians or Alaskan Natives, those having less than a high school education, and those with an annual family income of less than $25,000. These findings may reflect the known impact of alcohol dependence on many areas in the drinker’s life, including their ability to work and their productivity in the workplace. Reduced workplace productivity is the single largest contributor to alcohol-attributable economic costs in the United States (1). "The strong relationship between the prevalence of excessive drinking and binge drinking is also consistent with the findings of previous studies (17), as is the higher prevalence of alcohol dependence among binge drinkers relative to all current drinkers (8), and the positive relationship between the frequency of binge drinking and alcohol dependence (18). These findings emphasize the usefulness of screening for binge-level alcohol consumption to identify excessive drinking among adults, including those who are alcohol-dependent (19). The relatively low prevalence of alcohol dependence among people who drink excessively also suggests that most people who are screened for excessive drinking in clinical settings will probably not need to be referred for specialized treatment." Esser MB, Hedden SL, Kanny D, Brewer RD, Gfroerer JC, Naimi TS. Prevalence of Alcohol Dependence Among US Adult Drinkers, 2009–2011. Prev Chronic Dis 2014;11:140329. DOI: dx.doi.org/10.5888/pcd11.140329 |
| 10. Changes in Criteria for Identifying Cannabis Dependence: From DSM-IV to DSM-V "Based on NSDUH estimates, rates of cannabis abuse and dependence remained relatively stable from 2002 to 2019, with the highest rates of abuse and dependence among young adults (aged 18–25) (Figure 3-27). For 2020, except for youth (aged 12–17), for whom the data suggest a slight decline in rates of cannabis abuse and dependence, the data are generally consistent with the longer-term trends for the other age groups. In 2021, the NSDUH introduced the diagnostic category of cannabis use disorder to better accord with DSM-V criteria for classifying substance use disorders. The frequency of the disorder is higher than previous estimates of cannabis use and dependence (online Appendix E). Given that cannabis use disorder has only been measured for two years using the new DSM-V criteria, it is challenging to determine how this has changed over the full 20-year time period. It follows a similar pattern as that of cannabis use and dependence, with the highest rates of the disorder among young adults (aged 18–25), males, non-Hispanic American Indians/Alaska Natives, people living in poverty, and people with some college education. In 2022, cannabis use disorder was less common in pregnant persons than in the general population but was increasing in both populations (Figure 3-28, online Appendix E)." National Academies of Sciences, Engineering, and Medicine. 2024. Cannabis Policy Impacts Public Health and Health Equity. Washington, DC: The National Academies Press. doi.org/10.17226/27766. |
| 11. Risk of Heroin Dependence After Onset of Use "When observed within approximately 1 to 12 months after heroin onset, an estimated 23% to 38% of new heroin users have become dependent on heroin. Rank-order correlation and post hoc exploratory analyses prompt a hypothesis of recently increased odds of becoming dependent on heroin. "Seeking estimates for comparison, we found 3 published studies on how often heroin dependence was found among people who have used heroin at least once in their lifetime. The National Comorbidity Survey (1990-1992) estimate was 23% dependence rate (with a standard error [SE] of 5%); National Epidemiologic Survey on Alcohol and Related Conditions (2001-2002) estimate (SE) was 28% (4%); and National Epidemiologic Survey on Alcohol and Related Conditions-III (2012-2013) estimate (SE) was 25% (2%).4,6 These 3 values yield a random-effects meta-analysis summary of 26%, with a 95% CI of 22% to 29%, which clearly overlaps this study’s overall finding of 23% to 38% of all participants becoming heroin dependent soon after first heroin use." Rivera OJS, Havens JR, Parker MA, Anthony JC. Risk of Heroin Dependence in Newly Incident Heroin Users. JAMA Psychiatry. Published online May 30, 2018. doi:10.1001/jamapsychiatry.2018.1214 |
| 12. Probability of Transition From First Use to Dependence For Various Substances "In a large, nationally representative sample of US adults, the cumulative probability of transition to dependence was highest for nicotine users, followed by cocaine users, alcohol users and, lastly, cannabis users. The transition to cannabis or cocaine dependence occurred faster than the transition to nicotine or alcohol dependence. Furthermore, there were important variations in the probability of becoming dependent across the different racial-ethnic groups. Most predictors of transition were common across substances. "Consistent with previous estimates from the National Comorbidity Survey (Wagner and Anthony, 2002a), the cumulative probability of transition from use to dependence a decade after use onset was 14.8% among cocaine users, 11.0% among alcohol users, and 5.9% among cannabis users. This probability was 15.6% among nicotine users. Furthermore, lifetime cumulative probability estimates indicated that 67.5% of nicotine users, 22.7% of alcohol users, 20.9% of cocaine users, and 8.9% of cannabis users would become dependent at some time in their life." Catalina Lopez-Quintero, et al., "Probability and Predictors of Transition From First Use to Dependence on Nicotine, Alcohol, Cannabis, and Cocaione: Results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC)," Drug and Alcohol Dependence, 2011 May 1; 115(1-2): 120-130. doi:10.1016/j.drugalcdep.2010.11.004 |
| 13. Estimated Prevalence of Cannabis Dependence "Some 4.3 percent of Americans have been dependent on marijuana, as defined in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR; American Psychiatric Association, 2000), at some time in their lives. Marijuana produces dependence less readily than most other illicit drugs. Some 9 percent of those who try marijuana develop dependence compared to, for example, 15 percent of people who try cocaine and 24 percent of those who try heroin. However, because so many people use marijuana, cannabis dependence is twice as prevalent as dependence on any other illicit psychoactive substance (cocaine, 1.8 percent; heroin, 0.7 percent; Anthony and Helzer, 1991; Anthony, Warner, and Kessler, 1994)." Budney A, Roffman R, Stephens R, Walker D. Marijuana dependence and its treatment. Addiction Science and Clinical Practice. 2007;4(1):4–16. |
| 14. Admissions to Treatment for Marijuana in the US According to the Substance Abuse and Mental Health Service's Treatment Episode Data Set, in 2020 in the US there were 139,481 admissions to treatment with marijuana reported as the primary substance out of the total 1,416,357 admissions to treatment in the US for those aged 12 and older for all substances that year. By comparison, in 2010 in the US there were 358,034 admissions to treatment with marijuana reported as the primary substance out of the total 1,928,013 admissions to treatment in the US for those aged 12 and older for all substances that year. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. Treatment Episode Data Set (TEDS): 2020. Admissions to and Discharges from Publicly Funded Substance Use Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2022. |
| 15. Alternative Analysis of the Relative Risk from MDMA Use "Nutt et al. (2007) attempted to compare the relative dangers of the main types of psychosocial drug, using a series of subjective rating scales. Heroin and cocaine were graded as the two most harmful drugs, whereas Ecstasy/MDMA emerged as one of the least harmful (18th out of 20). Unfortunately, it was unclear how this low harm rating score for Ecstasy/MDMA was given, as they cited no empirical research studies or reviews. Instead, Nutt et al. (2007) suggested that: ‘for drugs which have only recently become popular e.g. Ecstasy or MDMA, the longer term health and social consequences can only be estimated from animal toxicology at present’. Nutt et al. (2007) noted that the most pleasurable drugs tended to be the most problematic, and on the ‘intensity of pleasure’ scale, heroin and cocaine were given maximum scores of 3.0. In contrast, Ecstasy/MDMA was given an ‘intensity of pleasure’ score of 1.5, which was lower than cigarette smoking at 2.2. It is unclear why Ecstasy was rated as less pleasurable than smoking a cigarette, although the low pleasure score contributed to its low harm score. "Another question concerned drug injections, with Nutt et al. (2007) noting that ‘The potential for intravenous use is taken into account in the Misuse of Drugs classification and was treated as a separate parameter in our exercise’. Cocaine and heroin were given maximum scores of 3.0, whereas Ecstasy/MDMA was given a score of 0. Again, this did not accord with the empirical literature. In their survey of 329 recreational Ecstasy/MDMA users, Topp et al. (1999) reported that 54 (16%) had injected Ecstasy. MDMA injecting may be atypical and only occurs amongst the more experienced Ecstasy users, although this pattern would also describe cocaine. Most cocaine users never inject, and it is only found with experienced users. Hence, the injection score for MDMA should be similar to that for cocaine. Many of the other Ecstasy harm values in Nutt et al. (2007) were surprisingly low. With revised values based on the empirical literature, MDMA rises to the fifth most harmful drug (Parrott, 2009b)." Parrott, Andrew C., "Human Psychobiology of MDMA or 'Ecstasy': An Overview of 25 Years of Empirical Research," Human Psychopharmacology: Clinical and Experimental, 2013; 28:289-307. DOI: 10.1002/hup.2318 |
| 16. Ranking of Substances by Potential for Harm "Method: Members of the Independent Scientific Committee on Drugs, including two invited specialists, met in a 1-day interactive workshop to score 20 drugs on 16 criteria: nine related to the harms that a drug produces in the individual and seven to the harms to others. Drugs were scored out of 100 points, and the criteria were weighted to indicate their relative importance." "Findings: MCDA [multicriteria decision analysis] modelling showed that heroin, crack cocaine, and methamphetamine were the most harmful drugs to individuals (part scores 34, 37, and 32, respectively), whereas alcohol, heroin, and crack cocaine were the most harmful to others (46, 21, and 17, respectively). Overall, alcohol was the most harmful drug (overall harm score 72), with heroin (55) and crack cocaine (54) in second and third places." Nutt, David J Nutt; King, Leslie A; Phillips, Lawrence D, "Drug harms in the UK: a multicriteria decision analysis," The Lancet (London, United Kingdom: November 1, 2010) Vol. 376, p. 1558. |
| 17. Difficulties in Assessing "Problem" Marijuana Use "The issues of measurement and conceptualization described above in relation to efforts to screen for problematic or harmful cannabis use highlight the shortcomings of ‘one-size-fits-all’ approaches to screening. Our examination of the existing literature and of cannabis users from a general population study and from a mixed-methods study of adult, stable, socially integrated users suggests that many cannabis users who may otherwise meet the criteria for being at moderate risk for problematic use are nonetheless able to successfully integrate cannabis use into everyday life with few associated problems. Indeed, our findings advocate that regular use of small amounts of cannabis does not appear to increase an individual’s likelihood of experiencing problems, and it does not threaten one’s ability to function well and perform expected roles. Even so, the tools used to assess potentially harmful cannabis use invariably serve to classify almost all ‘regular’ users as problematic users." Asbridge M, Duff C, Marsh D, Erickson P. Problems with the Identification of ‘Problematic' Cannabis Use: Examining the Issues of Frequency, Quantity, and Drug Use Environment. Eur Addict Res 2014;20:254-267. |
| 18. Links Between Early Life Stress, Abuse, and Neglect, and Substance Use and Dependence "Exposure to early life stress, even to more severe forms such as physical and sexual abuse and emotional neglect, is common in the general population. The degree of risk for adult psychopathology tends to be correlated with the severity of childhood maltreatment and the number of childhood SLE [stressful life events]. An important causal pathway that links early life stress to the onset of psychiatric disorders is the altered homeostasis in the HPA [hypothalamicpituitary-adrenal] axis and the altered stress response circuitry that underlies many disorders including anxiety, depression, PTSD, and addiction. There appears to be a direct pathway from chronic stress exposure in prepubertal children via adolescent problem drinking to alcohol and drug dependence in early adulthood that is independent of family history. Of course, this can only occur in individuals exposed to the availability of alcohol or drugs. Early life stress may increase vulnerability to addiction through permanent effects on the expression of genes within the mesolimbic dopamine reward pathway. Early onset of problem drinking in stress-exposed children may exacerbate the deleterious effects on the developing brain. Since a large proportion of stress-exposed children do not go on to develop addiction, clearly resilience factors, including gene–environment interactions, are important. This review of the literature indicates that prevention should focus on early intervention in problem families to forestall maltreatment. Adolescence is a critically vulnerable time for the development of risky drinking habits, and this is an area where prevention, through the development of positive family, peer, and neighborhood-mediating factors, is vital. A holistic approach to the treatment of alcohol and drug dependence is essential since treatment is unlikely to be effective unless underlying impediments such as early life stress are recognized and addressed." Enoch, Mary-Anne, "The role of early life stress as a predictor for alcohol and drug dependence," Psychopharmacology (Heidelberg, Germany: July 2010) Vol. 214, No. 1. |
| 19. Cannabis and Dependence "People who develop problems with marijuana may indeed be different from those who do not, but this phenomenon has been observed with other substances of abuse. A comparison with alcohol use and dependence provides a case in point. The great majority of Americans have tried alcohol and continue to drink alcoholic beverages regularly. However, only an estimated 10 to 15 percent of alcohol drinkers develop problems, and only some of these problem drinkers seek treatment. This is also true of those who have tried cocaine or heroin (Anthony, Warner, and Kessler, 1994). "That said, the experience of dependence on marijuana tends to be less severe than that observed with cocaine, opiates, and alcohol (Budney, 2006; Budney et al., 1998). On average, individuals with marijuana dependence meet fewer DSM dependence criteria; the withdrawal experience is not as dramatic; and the severity of the associated consequences is not as extreme. However, the apparently less severe nature of marijuana dependence does not necessarily mean that marijuana addiction is easier to overcome. Many factors besides a drug’s physiological effects—including availability, frequency and pattern of use, perception of harm, and cost—can contribute to cessation outcomes and the strength of addiction. The low cost of marijuana, the typical pattern of multiple daily use by those addicted, the less dramatic consequences, and ambivalence may increase the difficulty of quitting. Although determining the relative difficulty of quitting various substances of abuse is complex, the treatment literature reviewed here suggests that the experience of marijuana abusers rivals that of those addicted to other substances." Budney A, Roffman R, Stephens R, Walker D. Marijuana dependence and its treatment. Addiction Science and Clinical Practice. 2007;4(1):4–16. |